Mexican Researchers Develop Organs-on-Chips Technology
Scientists develop "organs-on-a-chip" to revolutionize drug testing. These miniature devices mimic organ functions, allowing researchers to test drug efficacy on patient cells before prescription.
Scientists at the National Autonomous University of Mexico (UNAM) are advancing cutting-edge technology to grow miniature human organs on microchips, a breakthrough that could transform how drugs are tested and personalized treatments are developed for conditions ranging from brain diseases to heart disorders.
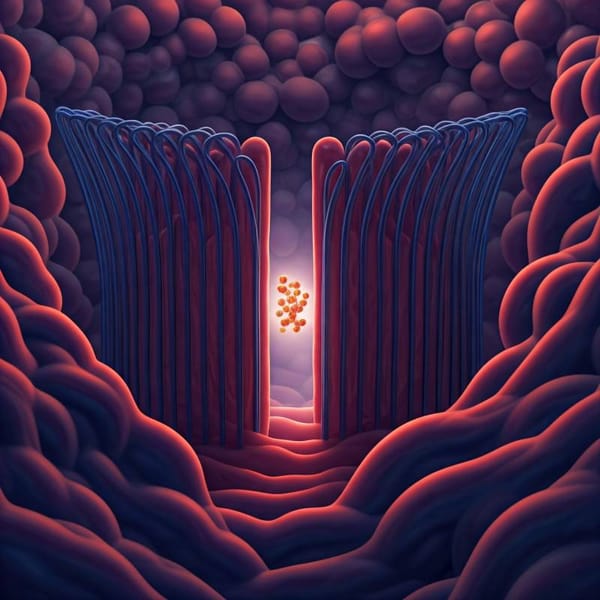
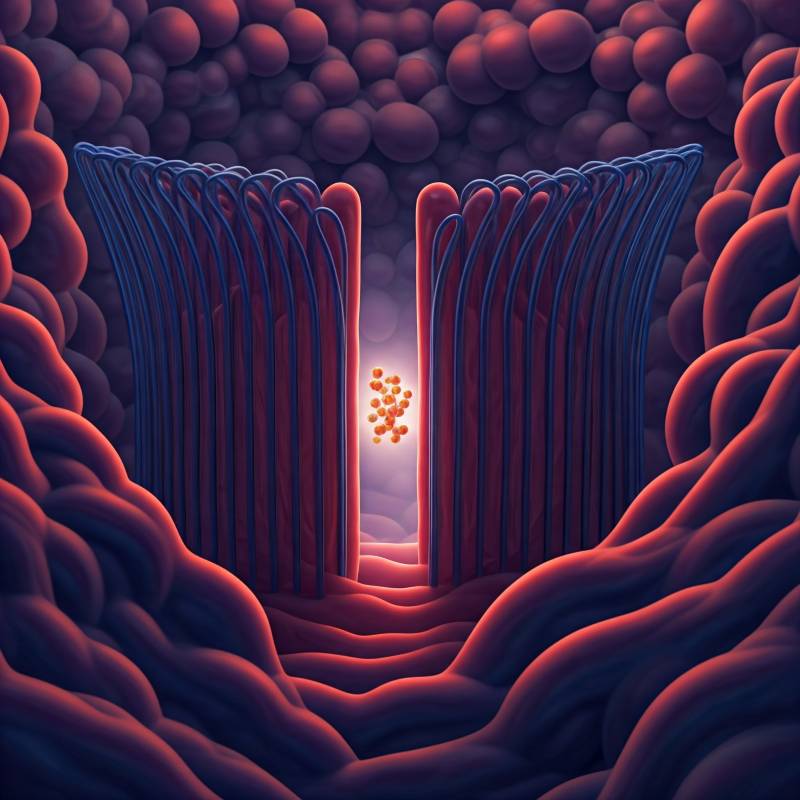
Led by researchers at UNAM’s National Laboratory of Biomimetic Solutions for Diagnosis and Therapy (LaNSBioDyT), the team is designing “organs-on-chips” (OoCs)—sophisticated devices that mimic the structure and function of human tissues. Their flagship project, a blood-brain barrier on a chip, aims to solve one of medicine’s most persistent challenges: delivering drugs effectively to the brain.
The Science Behind Organs-on-Chips
OoCs are 3D microfluidic platforms that replicate the mechanical and physiological conditions of living organs. Unlike traditional cell cultures, these chips allow cells to interact in environments that closely resemble human biology. Alejandra Maruri Sánchez, a researcher at UNAM’s Faculty of Sciences, explained that the devices are “transparent and versatile,” enabling scientists to observe cellular behavior in real time under a microscope.
“An organ-on-a-chip isn’t just a cluster of cells—it’s a functional unit,” said Maruri Sánchez. For instance, the team’s blood-brain barrier chip models the selective membrane that protects the brain from pathogens while permitting essential molecules like oxygen to pass through. This barrier involves complex interactions between endothelial cells, pericytes, and astrocytes, which the chip aims to replicate.
The blood-brain barrier project, spearheaded by Edda Lydia Sciutto Conde of UNAM’s Institute of Biomedical Research and doctoral student Nicolás Pérez Osorio, seeks to make this protective membrane more permeable to therapeutics. With brain diseases like Alzheimer’s and glioblastoma on the rise, the inability of many drugs to cross the barrier has stalled progress in treatment.
The chip features upper and lower compartments separated by a porous collagen membrane, simulating the interface where cells interact. “The goal is to test how medications can be transported more effectively to the brain,” said Maruri Sánchez, who helps engineer the microfluidic systems.
OoC technology could significantly reduce reliance on animal testing and costly clinical trials by predicting human responses to drugs earlier in development. Maruri Sánchez noted that these chips allow researchers to “evaluate new substances, review therapies, or test toxins” before advancing to human trials.
The potential for personalized medicine is equally compelling. By using a patient’s own cells, doctors could one day test drug efficacy on customized chips before prescribing treatments. “Humans are a system, not isolated organs,” Maruri Sánchez emphasized. Future iterations might link multiple organ chips to assess how a heart medication, for example, impacts the kidneys or liver.
While OoC technology is still emerging—pioneered less than a decade ago at institutions like Harvard’s Wyss Institute—UNAM’s work positions Mexico as a rising player in biotech innovation. Challenges remain, including scaling the complexity of human biology and securing investment for widespread clinical adoption.
Yet the promise is undeniable. “This isn’t just about building better models,” said Maruri Sánchez. “It’s about redefining how we approach treatments for every individual.” As global health demands grow more intricate, Mexico’s push to miniaturize human organs may soon deliver outsized breakthroughs.




Mexican scientists are shrinking lab work to microchip size—because bigger isn’t always better. Credit: UNAM